Market Access–Without the Guesswork
From formulary changes to rebate leakage, uncover what’s driving performance across payers, contracts, and patient access—with AI-powered speed and clarity.

Market Access is Complex. Analysis Shouldn’t Be
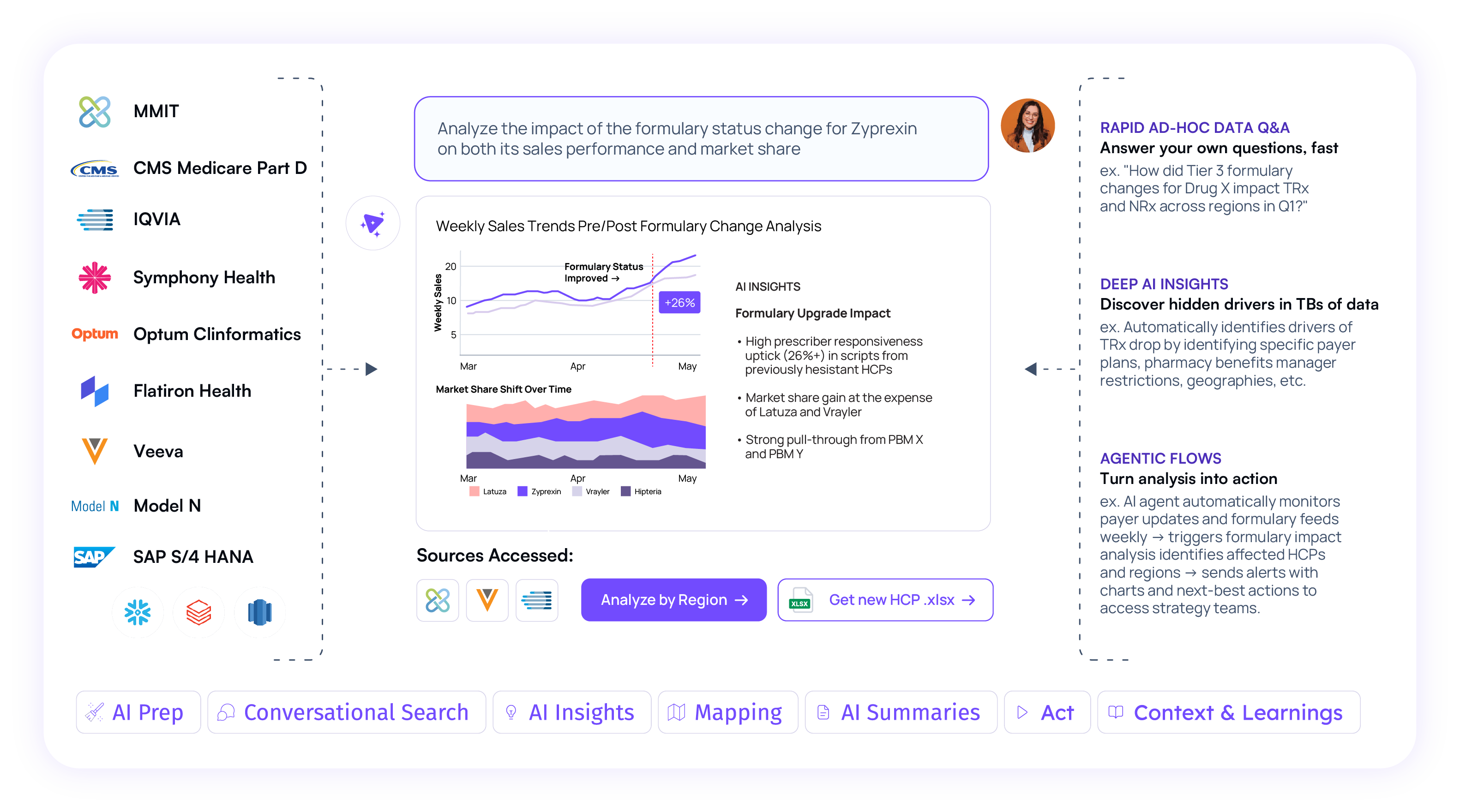
When formulary changes, rejected claims, or rebate mismatches hit, Market Access teams are expected to explain the “why.” But the data is fragmented, answers take too long, and critical opportunities are lost.

Claims, coverage, contract, and rebate data all live in different systems—making it nearly impossible to connect the dots. Answering a simple question like “Why did TRx drop?” takes days of manual stitching, if it’s even possible at all.

Rebate mismatches, late submissions, and over-utilized thresholds often go unnoticed until it’s too late. From NDC errors to missed forecasts, issues hide in siloed data—leading to lost value, compliance gaps, and fire drills that could’ve been prevented.

When access changes hit—like step edits, tier removals, or prior auth spikes—market access teams are expected to explain the impact fast. But delayed reporting means lost momentum, missed opportunities, and slow reactions when every day counts.
Unify Access, Rebate, and Payer Data. Get Answers in Seconds.
Tellius connects formulary, claims, contract, and rebate data into a single AI-powered workspace—so you can uncover what's driving TRx drops, flag non-compliance, and surface risks before they escalate.
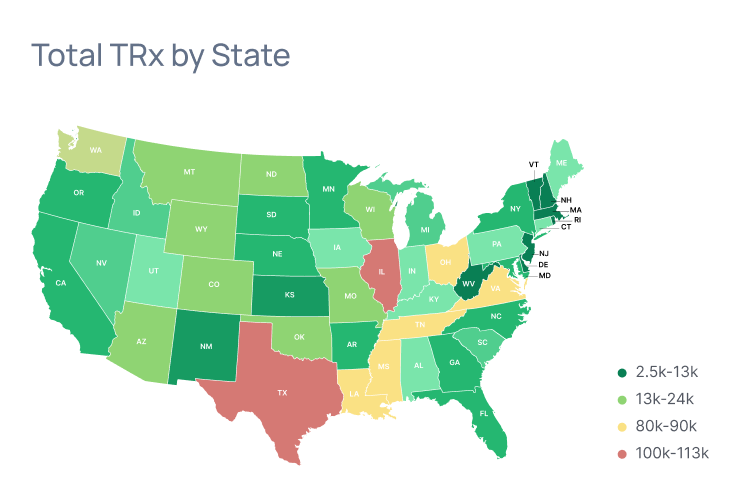
Don’t Let Coverage Shifts Catch You Off Guard
- Get proactive alerts when step edits, prior auth changes, or rejection spikes put access at risk
- Automatically monitor MMIT or plan-level updates across regions—no more waiting on static coverage reports
- See the TRx impact instantly by payer, geography, or segment—so you can act before it snowballs

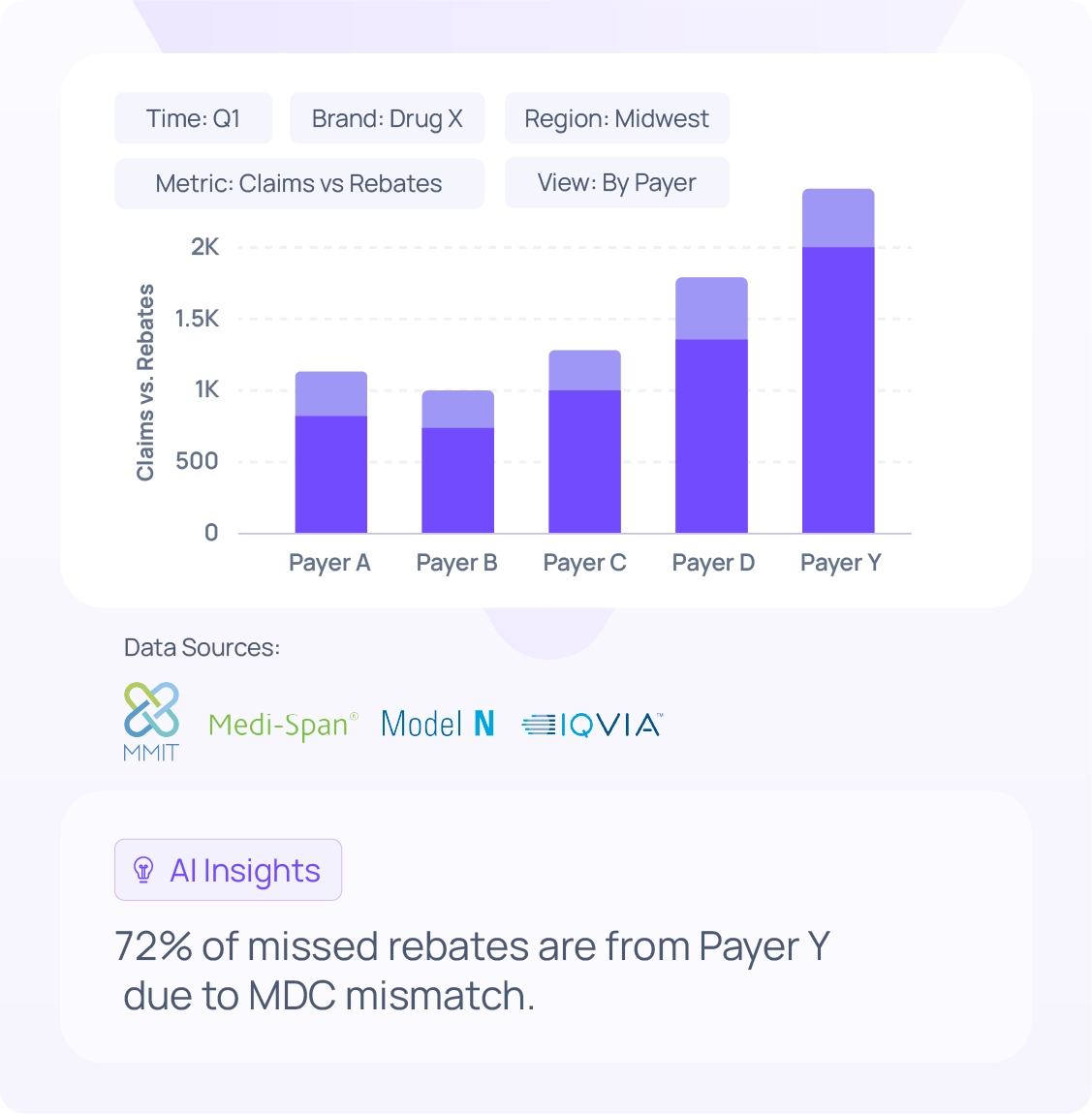
Spot Rebate Leakage Before It Hits the Bottom Line
- Uncover mismatches between claims and rebates paid—before dollars are lost
- Track contract thresholds and volume caps with automated alerts for overages and underutilization
- Compare forecasted vs. actual rebate payouts to catch issues and correct fast
Know What’s Driving TRx Change—Gain or Loss
- Detect brand erosion early with switch pattern analysis and abnormal drop-off alerts
- Measure pull-through impact by connecting Veeva activity to Rx performance
- Isolate access-driven changes by payer, plan, or campaign to guide next steps

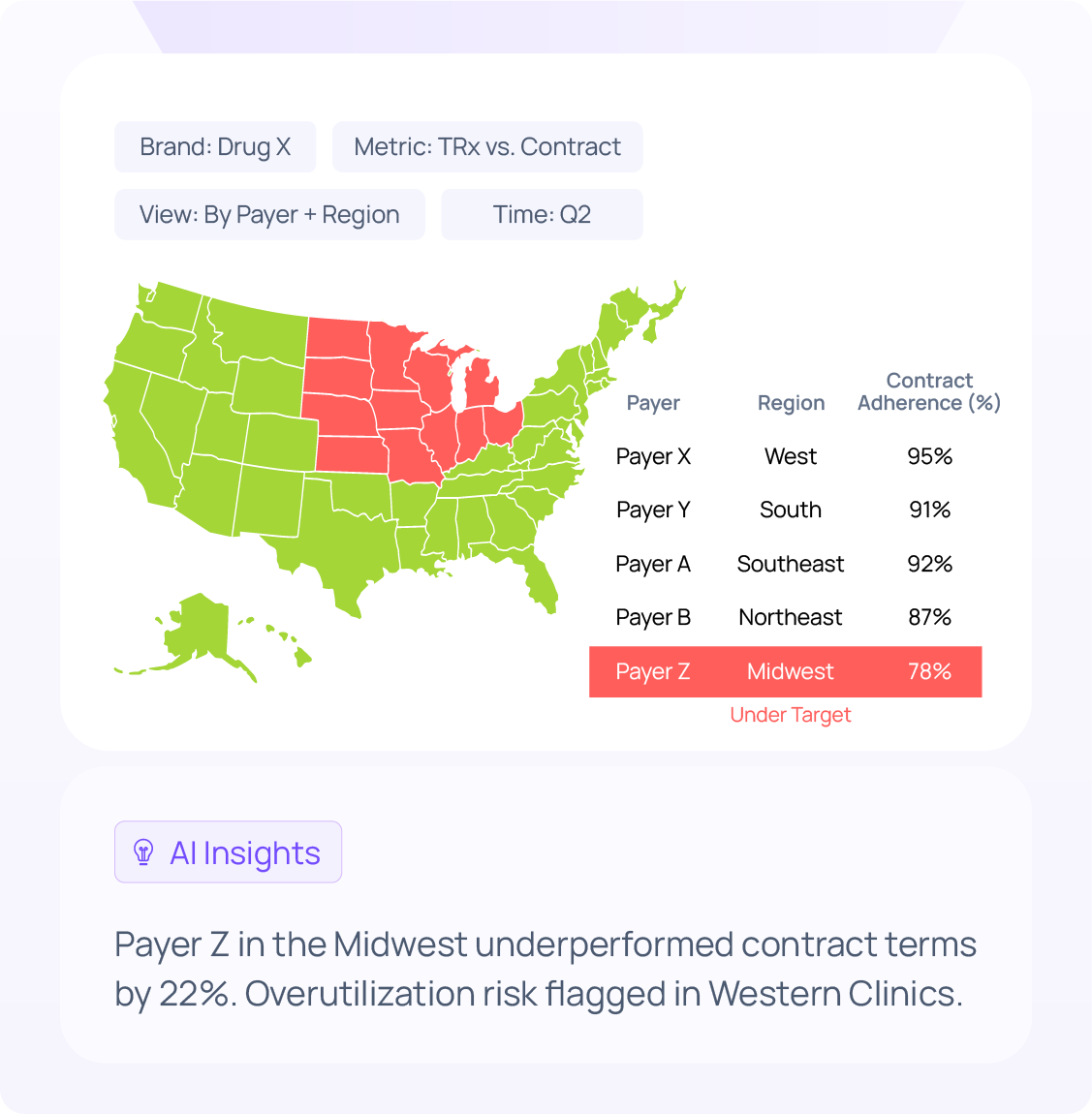
Map Risk and Opportunity by Payer, Geography, or Site
- Segment KPIs by territory and payer to uncover hidden performance gaps
- Identify contract compliance risks like overutilization or underperformance
- Align field, brand, and access strategy around local payer dynamics
Let AI Surface the Why—Before It Becomes a Fire Drill
- Trigger proactive alerts when TRx, rebates, or access KPIs deviate from baseline.
- Run pre-built workflows for coverage disruption, contract breaches, and rebate accuracy.
- Focus on action, not dashboards with always-on monitoring and guided root cause detection.

Let Your Data Tell You What’s Next — Before It’s Too Late
Tellius helps commercial, brand, and access leaders detect early signs of TRx slippage, uncover why it’s happening, and prioritize what to do next—without waiting on analytics teams.
Book a DemoAnswer + Act on Any Enterprise Question
& reporting
code-based predictive analytics
Conversations, Insights + Agentic Flows
Bring together internal & external data to drive pharma impact
Tellius connects data from IQVIA, Veeva, call activity, claims, and more—
to reveal what’s happening, why, and what to do next.
Trusted by 8 of the top 10 pharma companies to drive smarter decisions across field execution, brand performance, and access.
Conversational AI & Agents. Redefining Commercial Pharma Analytics.
Leave slow dashboards behind. Use AI-powered agents to uncover performance drivers, detect early warning signs, and prioritize commercial actions before competitors do.
Book a Demo














.png)